Diabetic Retinopathy
What is Diabetic Retinopathy
Diabetic retinopathy is the result of damage to the blood vessels in the eyes caused by diabetes. Since the blood vessels in the eyes and kidneys are the vessels most affected by diabetes, it is very likely that someone with diabetes for more than ten years will develop diabetic retinopathy.
The damage that occurs to the vessels in the retina causes a leak of fluid or blood, which then causes scar tissue to grow. This affects vision because the retina is the part of the back of the eye that detects light and visual images, and then transmits those images to the brain. Important blood vessels are located on the front of the retina, which get damaged as diabetic retinopathy develops. The leaking of fluid and blood, and the development of scar tissue then inhibit the retina’s ability to detect light and transmit images to the brain.
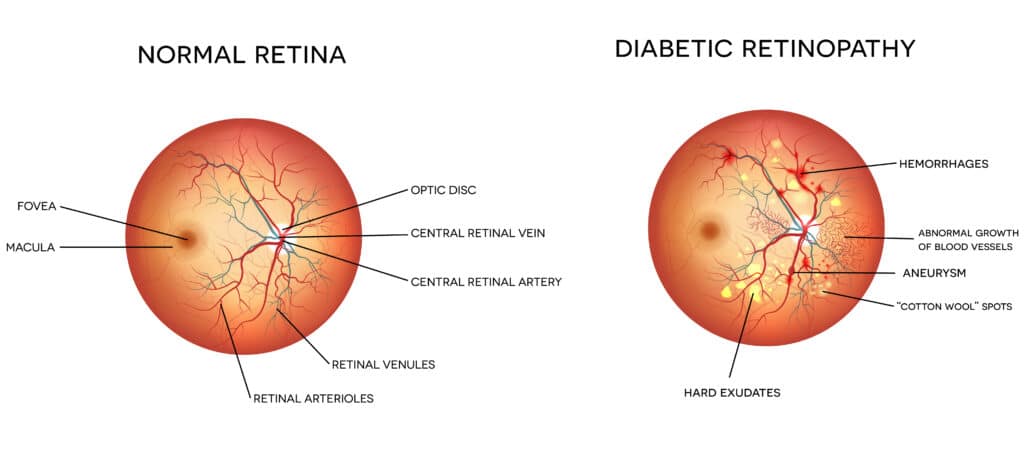
As diabetic retinopathy begins to develop, there are usually no perceptible symptoms. Near and far vision is typically unaffected at first. However, as the retinopathy advances, new blood vessels in the retina begin to grow as the eye attempts to replace the damaged vessels. Unfortunately, the new blood vessels the body generates do not function normally like the original vessels. These abnormal blood vessels may bleed and/or cause vision to become unclear, occasionally to the point of complete vision loss. Sometimes the abnormal vessels will cause the lens of the eye to develop cataracts, and if the vessels form on the iris of the eye they can cause glaucoma. Sometimes the newly formed vessels will cause scar tissue to form and can pull the retina from its proper location. This condition, called retinal detachment, if left untreated likely will lead to complete blindness.
While there are usually little to no symptoms of diabetic retinopathy in its earliest stages, there are some symptoms that start to appear as the disorder progresses. Seeing floaters, double vision, or other variations of vision loss are some of the most obvious symptoms, along with general difficulty reading or doing other work up close.
The main cause of diabetic retinopathy is diabetes.
While not everyone with diabetes will necessarily develop diabetic retinopathy, everyone with diabetes is certainly at high risk, especially those who have had diabetes for 10 years or more. Frequent changes in blood sugar increase the risk of developing diabetic retinopathy even higher. If you have diabetes, some ways to reduce the risk of diabetic retinopathy are monitoring and maintaining a controlled level of blood sugar and blood pressure, eating a healthy diet, exercising often and regularly, and getting an eye exam once a year to test for the changing of vessels in the eye. Even if you follow all of the ways to reduce risk of diabetic retinopathy, if you have diabetes it is imperative that you see an eye doctor regularly once a year to have a check up. This is the only way to catch the disorder early and to start treatment before significant vision loss has occurred. Your eye doctor will perform a fluorescein angiography in which colored dye will be injected into a vein and will travel through your body, including your eye. Your doctor will then take photographs of your eye through a colored filter to see if there is any damage to the retina lining or if there are any atypical blood vessels.
Treatment for diabetic retinopathy usually involves pan-retinal photocoagulation, a procedure in which a laser destroys all the dead areas of the retina. This causes the retina to stop creating new atypical blood vessels, and it usually causes the atypical vessels already present to decrease or even disappear completely. If cataracts have already formed from the diabetic retinopathy, then regular cataract removal surgery is usually performed to correct the problem.
